Research Highlights
- Aboriginal and Indigenous Health
Dr Sangita Sharma is a Centennial Professor and Endowed Chair of Aboriginal Health in the Faculty of Medicine and Dentistry at the University of Alberta and has over 22 years of experience working with multiethnic populations (eg Inuit, Inuvialuit and First Nations in Alberta, Northwest Territories (NT) and Nunavut (NU) and Alaska Natives, Apache and Navajo in the USA) focusing on chronic disease, diabetes and cancer prevention research. Sharma obtained her PhD from the University of Manchester Medical School in 1996 and since then she has worked with numerous populations in over 20 countries. Since moving to Canada in 2010, she has been leading a multi-disciplinary research group examining the risk factors for cancer, heart disease, diabetes, and obesity among Indigenous populations in Canada and around the world. As a Principal Investigator, Sharma has been awarded research funding for over 50 projects and was awarded the Silver Medal by the British Nutrition Society in 2010 for her health intervention program "Healthy Foods North" which was implemented in six communities in the NT and NU, in partnership with Inuit and Inuvialuit communities. Sharma has over 125 peer-reviewed scientific publications, including one recently in The Lancet Oncology (15:504-516, 2014) for her work studying cancer incidence in Indigenous populations through her Alberta Innovates-Health Solutions funded project "Cancer ACCESS", currently underway in the NT in Inuvik and Fort Good Hope. Currently, she is also running the "WHY ACT NOW" program in Edmonton to improve nutrition and physical activity in Aboriginal and new Canadian youth, funded in part by the Alberta Diabetes Institute. Other projects underway include the CIHR funded "MATERNAL" studying factors affecting pre- and post-natal maternal health in Northern Canada and NIH funded ASTHMA studies.
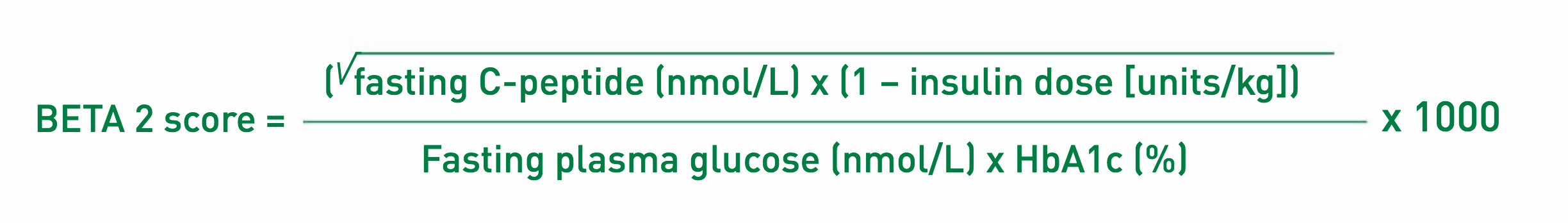
A better means of assessing islet transplant success - Since islet transplantations began taking place there has been 'scoring' of graft success, typically based on patient glycemic control parameters. Not surprisingly, the most accurate means of assessing graft performance are based on more complex metabolic measurements like mixed-meal tolerance tests (MMTTs) that are not as practical in routine clinical settings. Approaches that are too simplistic such as basic fasting glucose and C-peptide levels are confounded by exogenous insulin or poor gylcemia. To date, the BETA score has been most useful, and is essentially the arithmetic sum of scores (0 for diabetes range, 1 for intermediate, 2 for normal) for 4 components: fasting glucose, HbA1c, stimulated C-peptide and absence of endogenous insulin or oral hypoglycemic agent. However, this approach has limited sensitivity due in part to the categorical scoring of the parameters.Dr Peter Senior, Medical Director of the Clinical Islet Transplant Program, along with a team that included Dr James Shapiro and postdoctoral fellows Drs. Tolu Olateju and Richard Oram developed a new scoring system - the BETA 2 score. The basis of this score was continuous variables for common patient test values in a single, fasting blood sample - glucose, C-peptide, hemoglobin HbA1c and insulin dose. By using the measurements from 183 transplant patients that underwent MMTTs, and stepwise forward linear regression, the researchers were able to derive a mathematical formula for BETA 2 scores, with values over 20 reflecting insulin independence and scores under 15 reflecting glucose intolerance (see equation below).
In follow-up validation testing with 114 transplant recipients undergoing MMTTs 12 months after transplantation, BETA 2 scoring had over 82% sensitivity and specificity for correctly discriminating between these two groups. Results of this research show promise for the BETA 2 scoring system and warrant additional studies to validate its use (American Journal of Transplantation, doi:10.1111/ajt.13807, 2016).
- Innovative Obesity management
There is no ambiguity about obesity being a major risk factor for the development of T2D - what's worse, there is also a lack of proper weight management at the health delivery level by practitioners. Alberta Diabetes Institute scientists continue to make inroads in the fight against obesity at both the clinical and population health levels, including Dr Arya Sharma who is director of the Canadian Obesity Network (CON), Canada's largest association of healthcare professionals, researchers and policy makers working on obesity-related solutions. His own research focuses on evidence-based prevention and management of obesity and associated complications like diabetes. Sharma led the development of the 5A's of Obesity Management, a set of practical tools that can help guide health care professionals in weight management in primary care settings. Between 2013 and 2014 Sharma, along with Alberta Diabetes Institute member Dr Denise Campbell-Scherer and postdoctoral fellows Drs. Ayodele Ogunleye and Jody Asselin, conducted a controlled clinical trial to determine the effectiveness of the 5A's program in practice, collaborating with the Primary Care Network (PCN) of Alberta. The PCN is a front-line health care service in the Province, designed to bring local physicians together with mental health, dietary, nursing, pharmacy and other professionals to deliver integrative and comprehensive health solutions. The research helped health care providers identify their key knowledge gaps in regards to weight management intervention and the need for training for cultural, social and psychological factors. The result was a clear indication that most health care workers admitted they lacked the skills and confidence necessary to deal with patient weight management, and that training with 5A's intervention was effective in overcoming this shortfall. The 5A's intervention is a promising primary care-based approach for achieving better management of obesity that will be further assessed (BMC Research Notes, doi: 10.1186/s13104-015-1685-8, 2015). Meanwhile, fellow Alberta Diabetes Institute member Dr Geoff Ball is taking a similar approach to battling the rapidly growing health care threat of childhood obesity, which has increased nearly three-fold over the last three decades in Canada. Not surprising, overweight children become adults with similar weight challenges, making early intervention vital. A research team that included Dr Raj Padwal and PhD candidate Jill Avis explored how primary care providers use resources available to them to help manage juvenile obesity. Not surprisingly, their assessment revealed that most tools used by clinicians and parents were simplistic (eg, BMI) and focused on nutrition, with insufficient emphasis placed on contributing factors like physical activity and mental health. Ball and Avis created Resource Information for Parents on Lifestyle & Education (RIPPLE), a web-based tool that was easily accessible right in a doctor's waiting room. The idea was to have parents answer a series of questions about physical attributes and habits that would lead into a more informed discussion with their clinician. This tool was utilized in a pilot study at a PCN clinic, garnering highly positive feedback as well as areas for improvement. RIPPLE will be refined and tested further in the future (Telemedicine and e-Health, doi:10.1089/tmj.2015.0128, 2015).
