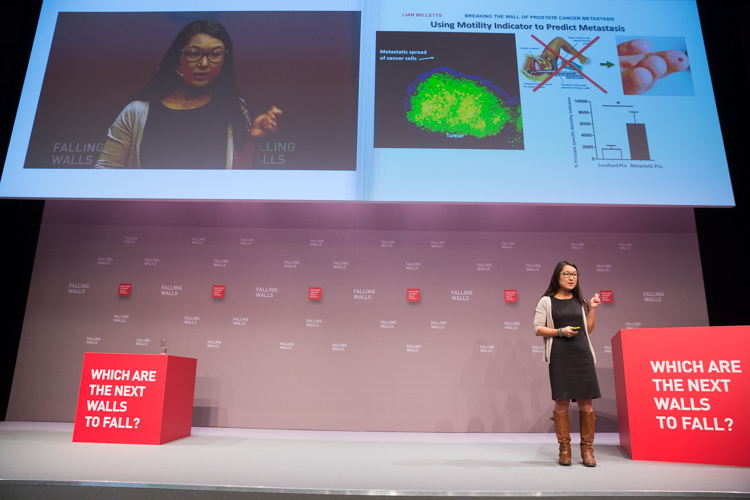
Lian Willetts presents at Falling Walls Lab
Throughout her life, Lian Willetts has always known she wanted to make a difference. But it wasn't until she lived through a difficult life event eight years ago that she determined where she'd make her mark.
"My mom died of cancer. She was diagnosed with a pain in her sacrum, but she died from lung cancer," Willetts says of her attraction to the field of oncology. "Resolving the issue of metastasis is dear and close to my heart. She wouldn't have passed away if it didn't spread."
Today, the post-doctoral fellow in the Faculty of Medicine & Dentistry's Department of Oncology is more determined than ever to help in the global fight against cancer-and she's succeeding. Her innovative work to identify patients at greatest risk of prostate cancer cells spreading to other parts of the body has earned her a top-two finish at the Falling Walls Lab finale in Berlin, Germany-a showcase of the world's best up-and-coming research talent.
"I feel extremely honoured and really supported," says Willetts. "Being able to be acknowledged by the jury and my peers that our project would have a meaningful impact in the future was an extremely rewarding and exciting experience."
Willetts was one of two Faculty of Medicine & Dentistry researchers at the event, and one of three in total representing the University of Alberta, out of a field of 100 scientists from around the globe. As part of her prize, she had the opportunity to present in front of 700 guests on the large stage of the Falling Walls Conference, sharing the spotlight and attention with Nobel laureates and groundbreaking researchers from all disciplines of science.
Willetts' award-winning efforts have enabled the creation of a simple blood test to predict whether patients have aggressive and invasive or non-aggressive prostate cancer. The new method is far less invasive than the current standard of care-undergoing a biopsy.
"Men don't die from prostate cancer. They die when the cancer starts to spread," says Willetts. "Using our technology and platform, we have been able to identify a lot of the indicators that would reveal the state of your cancer and if it will spread. In this sense we can provide a very accurate and predictive technology for patients who will be diagnosed with prostate cancer. This paves the way for increased survival, and most importantly, the quality of life of these patients."
Willetts, along with her mentor John Lewis, the Frank and Carla Sojonky Chair in Prostate Cancer Research at the U of A, are now honing the test to better determine its predictive accuracy over a longer time in much larger cohorts of patients from prostate cancer centres around the world. If all goes well, they hope to have it available for clinical use in the next few years.
"There are many men out there who get a diagnosis of prostate cancer that never would have killed them, but they still opt for radiation or surgery," says Lewis. "This can severely compromise their quality of life. I think the biggest benefit of this test will be in determining which patients can feel comfortable making the decision to forgo aggressive treatment and just monitor their disease to live with it over the long term."
This is the second year in a row that a U of A researcher has placed in the top two at the international competition. Willetts believes the results speak to the quality of work being done at the university.
"We are in a great environment to let our ideas fly, and it's a credit to the university. The U of A is definitely a leading force in research and innovation."
Breaking the wall of genetic medicine
Willetts' prize-winning work wasn't the only Faculty of Medicine & Dentistry research turning heads in Berlin. Joshua Lee, a PhD candidate in the Department of Medical Genetics, made an impression with his work developing new therapeutic strategies for treating genetic diseases-with a specific focus on Duchenne muscular dystrophy.
 "Our lab discovered we can use synthetic DNA-like molecules to affect the way the cells of the body, specifically in patients with muscular dystrophy, interpret their genetic code," says Lee. "These patients have a genetic mutation which prevents them from making a protein that is essential for muscle cell integrity. So we used these DNA-like drugs to cause the cell's machinery to skip over or ignore the mutations that are present, allowing the cell to produce the essential protein."
"Our lab discovered we can use synthetic DNA-like molecules to affect the way the cells of the body, specifically in patients with muscular dystrophy, interpret their genetic code," says Lee. "These patients have a genetic mutation which prevents them from making a protein that is essential for muscle cell integrity. So we used these DNA-like drugs to cause the cell's machinery to skip over or ignore the mutations that are present, allowing the cell to produce the essential protein."
"The approach that I developed specifically focuses on a region of the gene that is responsible for Duchenne muscular dystrophy. This new approach can treat about 45 per cent of all patients with this disease, whereas current clinical trials using the same kind of technology are only able to target about 13 per cent of patients."
Lee says his experience at the Falling Walls Lab was invaluable, allowing him to collaborate with other bright minds from around the globe and make important connections. His next step is to continue developing his therapeutic approach to Duchenne muscular dystrophy-which he believes could be applied to many other genetic diseases as well-with an aim of progressing it to clinical trials in the not-too-distant future.