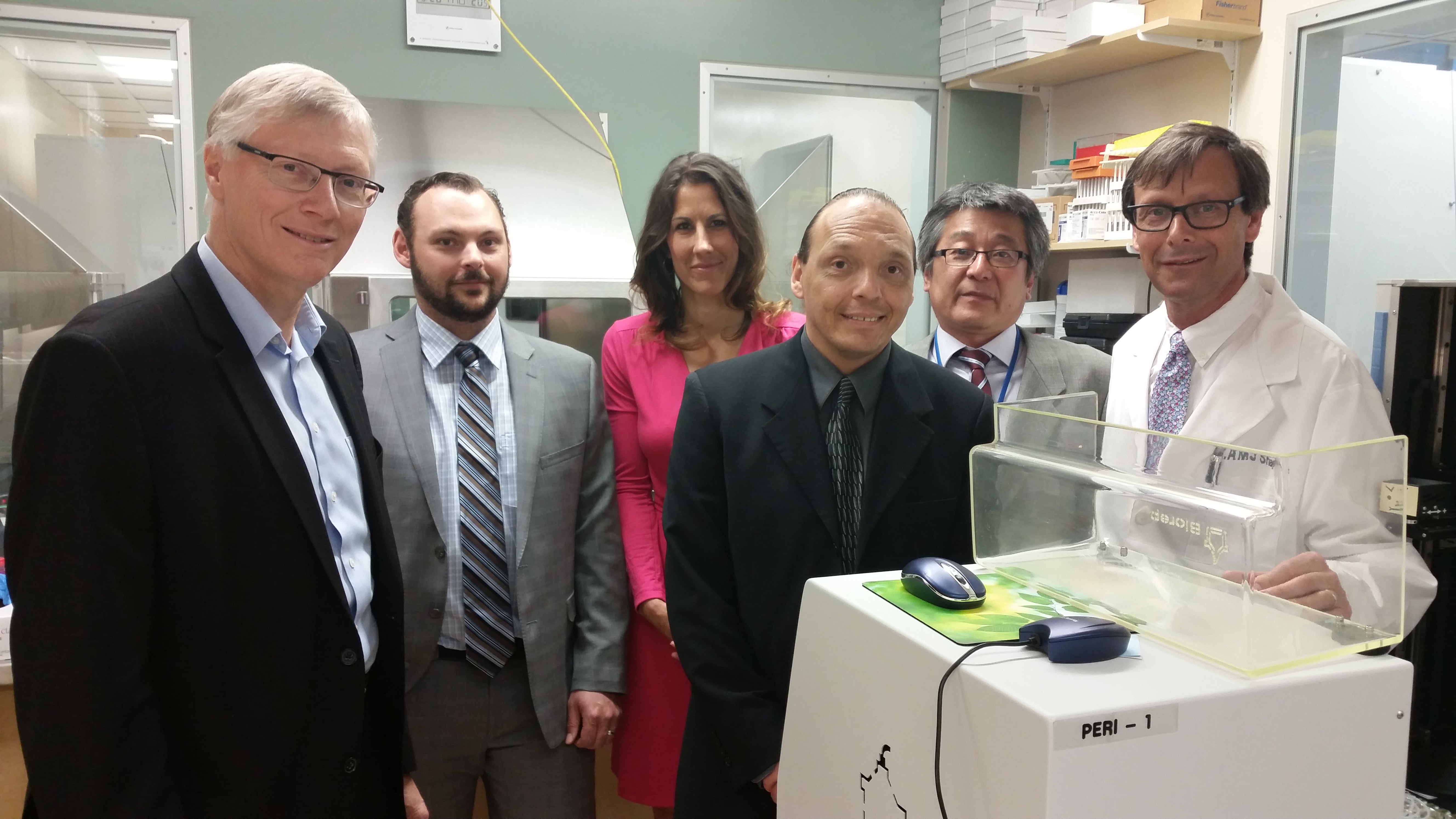
James Shapiro (on right) with members of his team along with islet cell transplant recipients Verlyn Olson, Allyson Hadland, and Jason Surgenor.
A local health-care team has cemented its status as global leaders in a groundbreaking diabetes treatment.
The team recently performed its 500th islet cell transplant, which helps people with Type 1 diabetes control their blood glucose levels without daily insulin injections.
"No other program has accomplished anything of this magnitude," says James Shapiro, Canada Research Chair in Regenerative Medicine and Transplantation Surgery and director of the Clinical Islet Transplant Program in the Faculty of Medicine & Dentistry. "We are international leaders in the treatment of diabetes because of this program."
The Edmonton Protocol, developed by Shapiro and his team at the Faculty of Medicine & Dentistry, involves isolating islet cells from a donated pancreas and transplanting them via non-surgical injection into the liver of an insulin-dependent recipient with severe Type 1 diabetes.
The donor islet cells produce insulin, which helps the transplant recipient regain control of their blood sugar levels, eliminating or greatly reducing the need for insulin injections.
Recipients typically undergo one or two transplants, and most patients experience a dramatic decrease in insulin requirement one month after a transplant.
About 225 patients have undergone one or more transplants since the faculty and Alberta Health Services established the program in 1999. Most of these patients have been able to stop insulin therapy for sustained periods, about half remain insulin free long term, and many others require small amounts of insulin to keep their blood sugar under control.
"Dr. Shapiro's research involving islet transplantation at the University of Alberta has been nothing short of remarkable," says Richard Fedorak, interim dean of the Faculty of Medicine & Dentistry.
"His expertise in establishing the Edmonton Protocol and his continual efforts to improve upon it are giving hope to patients with Type 1 diabetes around the world. It's with pride I can say that hope is being rewarded, as demonstrated through important milestones such as this."
To be eligible for treatment, patients must be 18 years of age or older with difficult-to-manage Type 1 diabetes, requiring multiple insulin injections every day. Most patients who've undergone the treatment had experienced blackouts due to poor blood sugar control.
Verlyn Olson, 62, was first diagnosed with Type 1 diabetes when he was 28 years old. Last fall, he was injured as a result of undetected low blood sugar, an episode he describes as a wakeup call. This year, he has undergone two islet cell transplants and today he is insulin free.
"I had been on an insulin pump for about three and a half years, but I was having a hard time identifying my lows," says Olson, a former minister with the Government of Alberta. "I was having to set an alarm in the middle of the night to check my sugars."
He says the Edmonton Protocol has restored freedom.
"I still feel weak from the anti-rejection medication but it is a small price to pay for the feeling of freedom and the control I have now," he says.
Shapiro and his team continue to innovate. For the 500th transplant, they collaborated with the University of Pittsburgh in pilot clinical research trial, which involved transplanting the cells under the lining of the stomach rather than in the liver. The patient, an Edmonton man, was the first in the world to receive islets injected into the stomach; the new approach enables physicians to see and biopsy the cells following transplant.
"The treatment we can offer patients today is a very good treatment but it's not a cure," says
Shapiro. "There is always room for improvement and we need to work hard in the lab and continue to make progress. Our team's goal is to drive research today to accelerate a cure for tomorrow."