Researcher identifies key elements for delivering quality primary health care in Alberta
As a health policy and systems researcher, Stephanie Montesanti seeks to understand the diverse health experiences people have. Through her work as a founder of Imagine Citizens Collaborating for Health, she is committed to working with patients, families and caregivers to envision a renewed health system for delivering high quality, culturally-resonant and safe care.
Imagine engages with Albertans in an effort to influence how the province’s health-care system works. The collaborative does this in four strategic ways, including:
- connecting and working with citizens to create a collective voice,
- identifying, assessing and reporting back on what matters to Albertans,
- collaborating with health-system providers to drive change, and
- gathering and sharing information to improve patients’ experience and results.
Montesanti worked with partners at Imagine on a Primary Health Care Project (PHC Project) that engaged with Albertans from across the province. The team listened to participants’ experiences and relationships along their primary health-care journey to report back to Alberta Health about how care is delivered in communities.
Primary health care is a patient’s first point of contact for treatment and management of a health condition or to receive health and wellness advice. In Alberta, primary health care is delivered in a variety of settings, including community health centres, family care clinics, and primary care networks (PCNs) member clinics.
Primary health care initiatives in Alberta have supported the establishment of a medical home for Albertans to provide coordinated, integrated and patient-centred care. The concept of the medical home was first developed in the United States in 1967. The aim is to improve the coordination of primary care and to place greater emphasis on the needs of patients with an orientation towards the whole person.
“While a house is a place of residence or refuge, the term home is often used in a more personal and emotional way. It can be an environment characterized by security, safety and happiness,” explains Montesanti.
From their engagement with diverse Albertans, Montesanti and colleagues captured three key elements of a new health home model needed to provide continuous, quality care.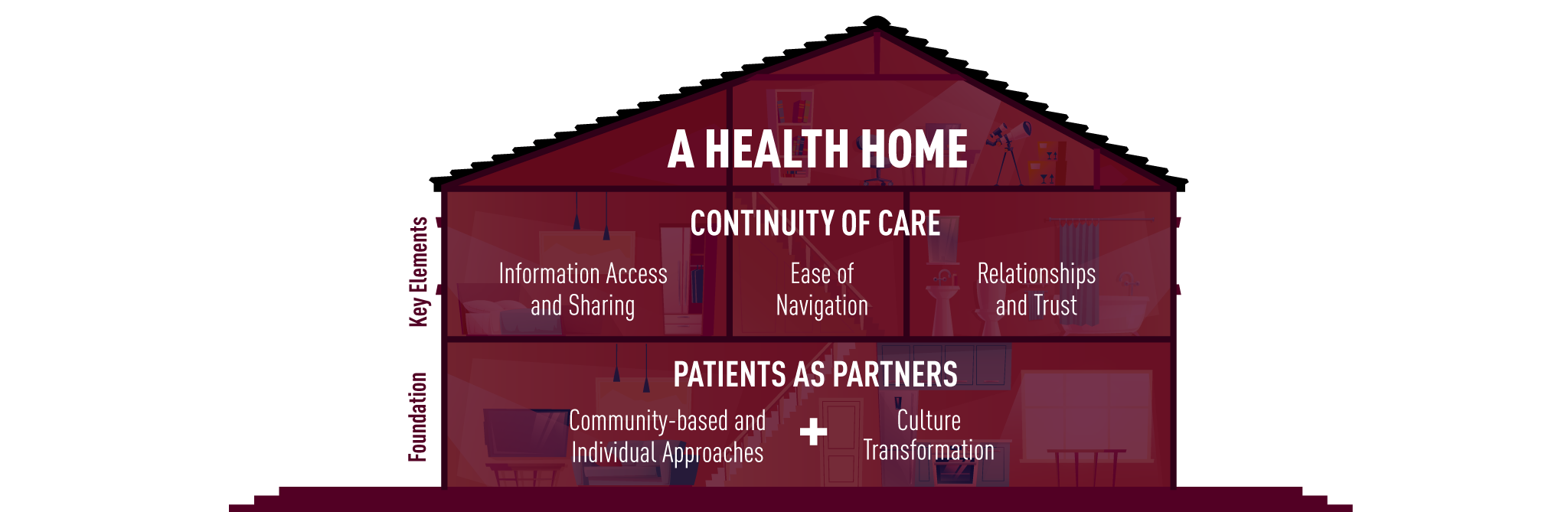
Information access and sharing
By being a patient of a health home, patient information is shared between providers.
“Information sharing between allied health professionals is especially helpful for patients managing chronic conditions, which often co-exist and require multiple health providers and access to services,” explains Montesanti.
Additionally, with access to their own health records, patients are better informed and can take more responsibility for understanding, monitoring and directing their own health.
Ease of navigation
“With an interdisciplinary team of physicians, nurses, mental health workers, dietitians and others, there is improved coordination of care and continuing navigation of care,” Montesanti says. “This prevents patients, especially those with complex health needs, from falling through the cracks.”
“If a patient has a language barrier, or is unfamiliar with our health system, it’s especially challenging to navigate their health journey,” Montesanti says.
According to Montesanti, hiring community health navigators who act as a single point of contact for patients needing support for making appointments, attending appointments with them and managing transportation is one intervention to assist patients with health system navigation.
Currently, Montesanti is working in partnership with PCNs in Edmonton to implement a community health navigator program more widely.
Relationships and trust
“When a patient becomes attached to a primary care physician and clinic it can facilitate a constant and ongoing relationship with a single provider,” explains Montesanti.
“However, Albertans that were engaged in the project expressed negative feelings towards the word ‘attachment’, and instead emphasized the importance of relationships and trust with their health-care team.”
Albertans expressed a desire for flexibility to change to a primary care physician and clinic that was right for them. They described positive relationships with physicians and practitioners who valued their patients, and took time to listen and understand their unique situations and needs.
Patients as the foundation of the health home
“The foundation of the health home model needs to be patients as partners in their own care,” says Montesanti. “Both community and individualized approaches to health-care delivery and culture transformation are the building blocks.”
Specific communities have specific needs. “Primary care providers that are connected with community organizations and agencies and build partnerships across the sectors are better able to create solutions that promote health,” said Montesanti.
“Individually, patients want their health provider to recognize their personal situation and take an individualized approach to their care.”Stay in the know
Stay in the know with news and updates from the School of Public Health.