Carlene Johnson and Carla Prado conduct clinical research at the Alberta Diabetes Institute.
Leading up to World Diabetes Day on November 14, the University of Alberta recognizes the importance of raising awareness about the effects of diabetes on our communities, and the efforts of health professionals to improve patients' lives and find a definitive cure.
Whether it is type 1 or type 2 and the differences that come with each of them, diabetes is a chronic, complex disease that affects millions of Canadians every year. According to the Canadian Diabetes Association, 3.4 million Canadians are currently living with diabetes, at a cost to the health care system and economy of more than $11 billion a year.
The Alberta Diabetes Institute at the University of Alberta is spearheading multiple initiatives at the forefront of diabetes research, tackling the disease from every possible angle with the help of 62 research members from the faculties of medicine & dentistry, agriculture, life and environmental science, pharmacy and pharmaceutical sciences, physical education and recreation and the School of Public Health, as well as collaborating with the University of Calgary and Athabasca University.
Here are seven ways the Alberta Diabetes Institute's research and programs are making a difference:
1. Islet cell biology and physiology: From insulin dimmers to brain signals
Always looking for deeper knowledge of the human body and how diseases begin, researchers at ADI take big leaps to understand diabetes and find better ways to treat it.
Promising health researcher Jessica Yue looks into the role of the brain in the development of diabetes. Yue's investigation explains how the brain regulates fat metabolism and prevents cardiovascular disease, an important risk factor for obesity and diabetes. The signals sent by the brain to the body that usually protect a person from over-producing harmful lipids may fail sometimes, allowing a bigger risk for developing these diseases. Yue has opened a path to possibly prevent diabetes by identifying the potentially faulty process quickly and developing new therapies to intervene.
Killam 2016 Professorship recipient Patrick MacDonald and his team investigate the insulin 'dimmer switch,' a molecular pathway that regulates secretion of insulin on islet cells. The switch doesn't work in people with Type 2 diabetes but can be "turned back on" by restoring the pathway. By understanding islet cells and these pathways, researchers can find new ways to treat, delay or prevent diabetes.
2. Risk and prevention: Finding the guts to stop diabetes
The answers to why we get diabetes may be more than a gut feeling.
Jens Walter drives his research toward the differences of gastrointestinal microbiota among different populations of the world, and how our "westernized" diet and environment may impact the development of certain diseases like diabetes from the gut. Walter's field of research is an opportunity to discover new contributing factors to diabetes and novel ways to prevent it with adjustments to our daily habits.
Other research from Alberta Diabetes Institute for prevention cover areas like Prader Willi Syndrome, metabolic fat balance and cholesterol metabolism in diabetics.
3. Secondary diseases: Eliminating side risks
The treatment for one disease shouldn't be the cause for another.
Scot Simpson, Peter Senior, Dean Eurich and Alberta Diabetes Institute director Peter Light, along with PhD student Ahmed Abdelmoneim, are digging deeper into safety studies to try to find more clarity on the real cardiovascular effects of Sulfonylurea (SU) drugs, some of the first and-still-most popular treatments for type 2 diabetes. Their research on SU safety could lead to a better design of safety studies with more reliable data and trials that outline the risks and effects of diabetes medications.
Gavin Oudit, Gary Lopaschuk and their team work on a potential therapy that acts on the blood pressure regulation mechanisms of the body to prevent diabetic kidney disease or diabetic heart disease. More information on their research is in the journal Circulation: Heart Failure.
4. Immunology and cell therapies: Uplifting the islet success
After becoming the site of the first human islet transplantation in Canada, and later the development of the Edmonton Protocol by the U of A's Islet Transplantation Group, Edmonton continues to be a leading hub for islet transplantation and research.
Greg Korbutt is leading groundbreaking research to study the possibility of using porcine islets-instead of human islets, which are in limited supply-for cell replacement therapy on type 1 diabetes patients. His work also includes the creation of a 'matrix' with substances that could deliver nutrients to the islets and protect them from immune attacks, improving their chances of survival after transplantation.
James Shapiro, Peter Senior and Gina Rayat work simultaneously to find different approaches that increase islet survival and reduce cell injury during the process of transplantation.
5. Population health: Delivering the best patient care for specific needs
Part of the thorough work to manage treatment for type 2 diabetes is looking for strategies to make health care reach communities more effectively not only by delivering the right medications but also making sure that basic issues like patients' weight management are addressed correctly in primary care settings.
Arya Sharma leads the fight against obesity at both clinical and population health levels, with initiatives like the 5 A's of Obesity Management, a set of tools for health care professionals to improve their confidence and skills when treating patients that need help with their weight management.
Geoff Ball also focuses on this topic to prevent and manage childhood obesity, including important factors of its treatment beyond nutrition like mental health and physical activity.
Sanghita Sharma focuses her research on Aboriginal populations and their risk factors for cancer, diabetes and other diseases. She currently runs the WHY ACT NOW project to improve nutrition and exercise among Aboriginal and new Canadian youth.
Jeff Johnson, Chair of the Alliance for Canadian Health Outcomes Research in Diabetes (ACHORD), reviews the changes in health at the economic, clinical and humanistic levels. The vision is to develop and maintain a long-term, sustainable, multi-provincial research program to improve the overall quality of life of people with diabetes and lift the significant burden on Canada as a whole.
6. Up and coming research: Ensuring health in body and mind
The more brilliant minds we have looking for answers, the better results.
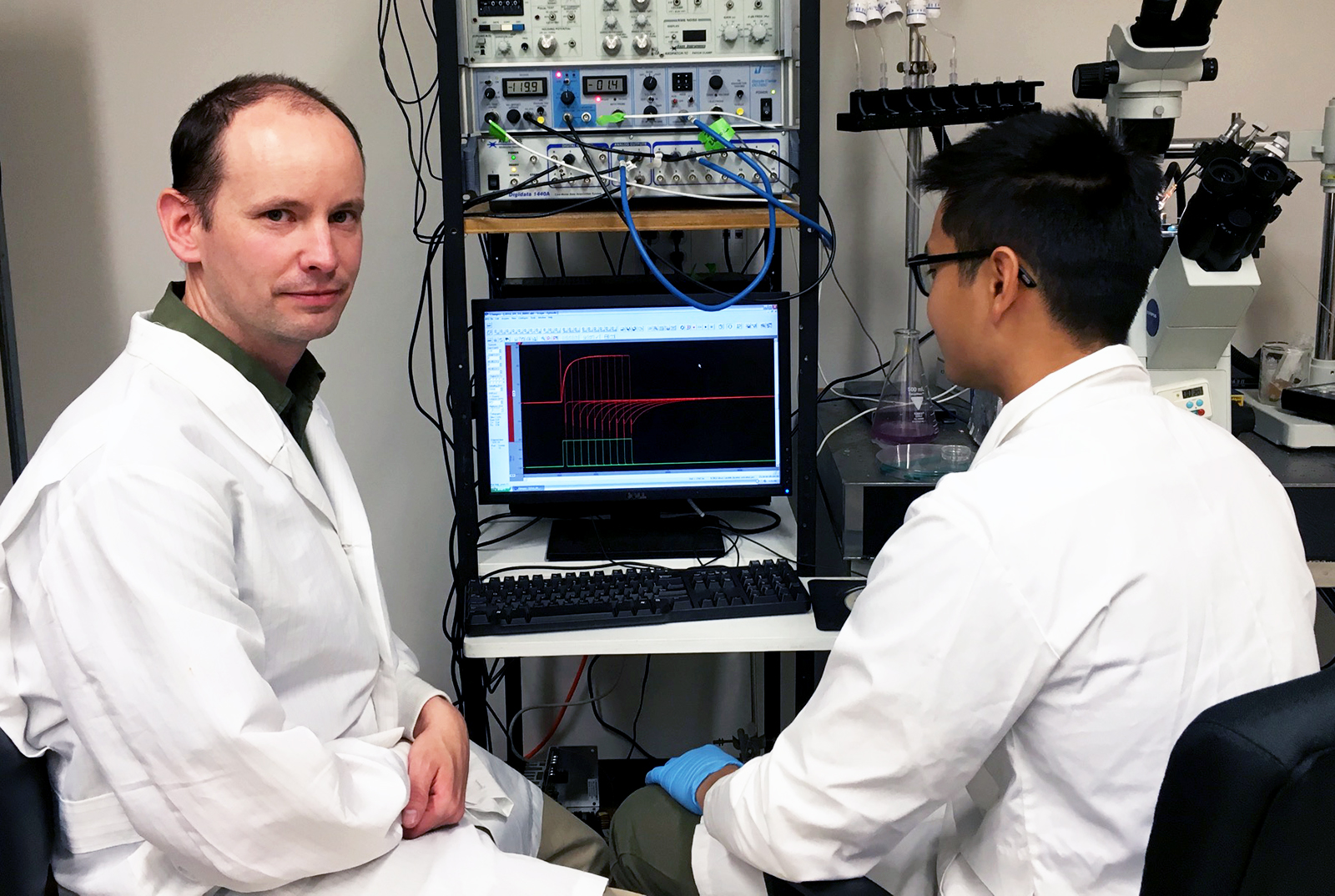
The Alberta Diabetes Institute keeps adding new and talented researchers to its front lines, like Harley Kurata. He studies how genetic mutations can affect regulatory mechanisms of insulin release, leading to an early development of diabetes in the first weeks or months of life.
His research also helps find new ways to care for and improve cognitive health on patients with diabetes. He delves into mechanisms of diabetic complications in the nervous system that may cause a higher prevalence of learning disabilities and other long-term mental issues in patients. Kurata's research tries to find the connection between metabolic disturbances in diabetes and the brain signals and proteins that could lead to the decline of these functions.
7. Facilities: Where science meets people
In 2017, the Alberta Diabetes Institute will celebrate 10 years in their home at the Li Ka Shing Institute for Health Research Innovation. But it is not just a place for researchers. The institute also facilitates clinical research in vital areas that impact the onset and management of diabetes including biomedical, nutrition and metabolism and physical activity. These help translate new ideas into proven therapies in patients.
The Clinical Research Unit, working in conjunction with the University of Alberta Hospital, runs phase II-IV clinical trials for new therapies involving patients. The Human Nutrition Research Unit supports the nutrition and metabolic areas of clinical research for truly integrated diabetes studies led by director, Carla Prado. This facility has state-of-the-art equipment for measuring body composition, including the Whole Body Calorimetry Unit-one of two in Canada-which is the most precise way to measure energy needs. There are fewer than 20 of these kinds of facilities in the world.
Meanwhile, the Physical Activity Diabetes Laboratory (PADL) gathers exercise physiologists that investigate the effect of physical activity-or lack of it-on type 1 and type 2 diabetes patients. Some of their most interesting research includes E-PAraDiGM (Exercise-Physical Activity Diabetes Glucose Monitoring) led by facility director, Norm Boulé (in photo, left) and the impact of physical activity on women at risk for type 2 diabetes, before and after giving birth.
More about the Alberta Diabetes Institute
The Alberta Diabetes Institute dedicates its facilities to the study of diabetes 'from bench to bedside,' translating health research into patient care solutions that improve the prevention, treatment and quality of life of type 1 and type 2 diabetes, as well as working to find a permanent cure.
Want to help prevent and cure diabetes? You can contribute by donating or participating in a clinical research study.
Photos: Alberta Diabetes Institute, Faculty of Medicine & Dentistry, www.whyactnow.ca.