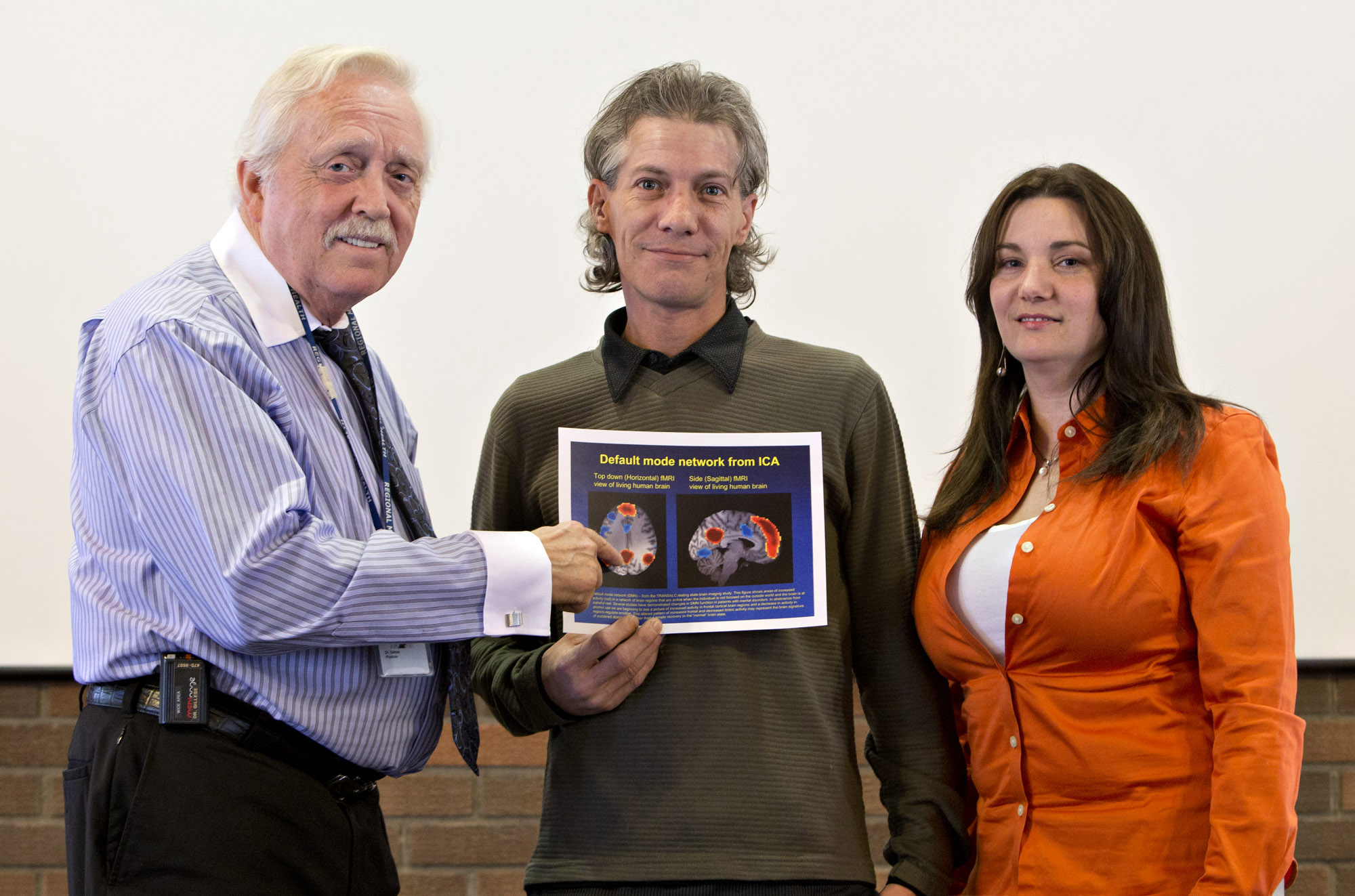
Research psychiatrist Dr. Tim Gillese, left, study participant Kirk Haakensen, and Henwood Treatment Centre Clinical Supervisor Jasmine Fulks with an MRI image of a brain scan used to tailor treatment for alcoholism.
"When it became too much, I just couldn't deal with it on my own any more and I realized I needed to get help," says the 43-year-old Edmonton musician. "I came to the Henwood Treatment Centre - and it was great."
As he successfully completed his residential program earlier this year, Haakensen also stepped up to take part in, and benefited from clinical research that uses brain imaging and drug therapy to better understand how microscopic changes in brain connectivity relate to alcohol dependence and recovery.
The TRANSALC project uses a magnetic resonance imaging scanner to take 'snapshots' of the brains of newly abstinent patients, then compares them to 'snapshots' taken a month later, to look for biomarkers, or signs, of how the human neural network begins to mend itself during recovery. Researchers aim to use brain imaging to develop personalized treatment and medication plans for problem drinkers.
"There's a host of literature on how alcohol damages the brain," says psychiatrist Tim Gillese. "Much less is known about how fast, or what the mechanisms are, for brain recovery.
"More recently, we've become aware of the genetics of how the drug naltrexone treats human alcoholism - and we're curious to know what changes take place in the brain with this drug that accentuate the recovery process, and how it extends the time between relapses."
Naltrexone is primarily used in the management of alcohol dependence and, since the early 1990s, a number of studies have confirmed its efficacy in reducing frequency and severity of relapse to drinking.
This research is a partnership between Alberta Health Services' (AHS) Henwood Treatment Centre and the Faculty of Medicine & Dentistry, University of Alberta. Groups within the university involved in the TRANSALC project include the Department of Psychiatry, the Neurochemical Research Unit, the Department of Biomedical Engineering and the Peter S. Allen MR Research Centre. With its adult residential treatment program, the Henwood assists with the recruitment of appropriate individuals to participate in the study.
"We've reached out to the university to make connections and found an affinity with its research department," says Jasmine Fulks, Henwood Clinical Supervisor. "This research is an important piece of the puzzle in filling in how alcohol addiction works - and how it can be treated."
Serdar Dursun leads the U of A team of Tim Gillese, Andy Greenshaw, Matthew Brown, Allan Aubry and clinical research nurse Marnie MacKay, who are the sole Canadian contributors to an international collaboration underway at sites in Germany, Finland and Spain.
"We hope to predict that a patient will do particularly well on an anti-alcohol pharmacological intervention," says Dursun, also a professor of psychiatry. "Then clinicians will be able to prescribe these medications, using a highly personalized approach, for the patient's benefit.
"Currently, we have no specific predictors, no markers, and our existing treatment options can be trial and error. Naturally, we want to avoid trial and error. We hope to come up with specific, selective neuromarkers, through imaging, which we can then use to make a particular, personalized decision on an individual's treatment."
Haakensen is one of about 20 participants who have been in the study for at least one month and two MRI scans.
"If there's anything I can do to help people with alcoholism, I owe that to the community. I'm happy to do it," he says. "The care has been outstanding. Those Henwood people are saints. They care about everybody there and they do whatever it takes to help each person as an individual. I was really impressed."
While research and recruitment are ongoing, early results are promising: 83 per cent of patients on naltrexone remained abstinent at one month and remained so at three months. For patients without naltrexone, only 56 per cent remained abstinent at least one month.
"I think this is a big advance in moving towards better continuity of care," says Greenshaw, professor and associate chair (Research) in the Department of Psychiatry. "We're interested in what happens in the brain in the short term when somebody stops drinking. Does the brain go back to normal? Does the brain change in a way that enables a person to stop?
"We're already seeing some early changes in brain pathways that relate to decision-making and to the reward system of intoxication. It's almost like you're turning down the rewards system and turning up the system that's responsible for inhibiting behaviour."
A Health Canada survey indicates 76.2 per cent of Albertans drink alcohol. Most who drink do so moderately and responsibly. However, when alcohol is misused, it can cause considerable harm to individuals and communities. Annually, alcohol abuse costs Albertans $855 million in lost productivity, $407 million in direct health care costs and $275 million for law enforcement.